views
Report Overview
U.S. Medical Coding Market size is expected to be worth around USD 44 Billion by 2032 from USD 20.3 Billion in 2023, growing at a CAGR of 9.4 % during the forecast period from 2023 to 2032.
The U.S. medical coding market is entering a transformative phase in 2025 as healthcare providers embrace AI-powered coding tools and strategic onshore outsourcing models. While ICD-11 adoption has boosted code precision and billing accuracy, rising claim volumes and stricter compliance demands are prompting hospitals and clinics to partner with domestic service providers offering on-demand coding across multiple specialties.
AI-assisted encoders and integrated workflow platforms are speeding coding processes, while coders shift focus from data entry to exception management and audit oversight. As federal pressure mounts for secure and interoperable coding practices, providers are investing in scalable, human–AI hybrid models that balance automation with quality control. This balanced deployment is expected to stabilize turnaround times, improve reimbursement accuracy, and reshape hiring—favoring coder–auditors skilled in technology oversight.
Click here for more information: https://market.us/report/u-s-medical-coding-market/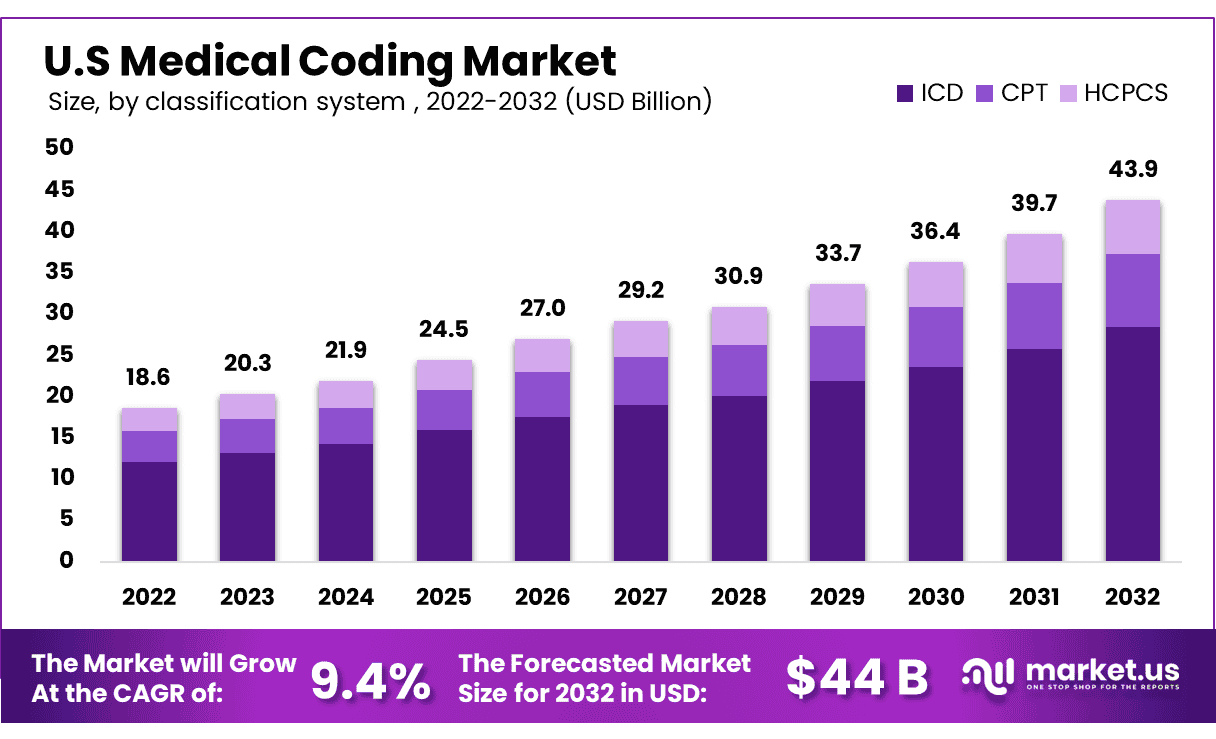
Key Market Segments
By Classification System
- ICD
- HSPCS
- CPD
By Component
- In-House
- Outsourced
- On-shore
- Off-shore
By Medical Specialty
- Emergency Services
- Oncology
- Anesthesia
- Cardiology
- Pathology
- Radiology
- Other services
Market Key Players
- StarTek
- Oracle
- Maxim Healthcare Services
- Parexel International Corporation
- Aviacode Inc.
- Verisk Analytics, Inc.
- Medical Record Associates, LLC.
- Optum
- Dolbey System Inc.
Get a Sample Copy of the Report to Know More: https://market.us/report/u-s-medical-coding-market/request-sample/
Emerging Trends
AI-first encoders are becoming standard in medical coding, automating routine tasks and flagging complex cases for human review. There's a notable shift toward onshore, just-in-time coding, where U.S.-based teams flexibly support seasonal or specialty spikes while keeping PHI within domestic regulations.
Coders are evolving into technology overseers—auditing AI outcomes rather than manually entering data. Finally, voice-to-text integration in EHR platforms is enhancing efficiency, leveraging natural language processing to reduce documentation time while maintaining accuracy.
Use Cases
Integrated AI-coding systems are now widely used in high-volume segments like cardiology, radiology, and emergency department billing—where multi-layered documentation and complex modifiers often trip up traditional workflows. AI flags inconsistencies and prompts coders for checks, reducing claim denials and reimbursement delays.
Hospitals also deploy coding pods during seasonal health surges or mass vaccination campaigns, scaling coder–auditor teams on demand. Telehealth visits benefit from AI pre-coding bots that prepare claim-ready documentation, lowering the manual lift and freeing coders to focus on specialized audits and provider education.
Contact us on
Market.us (Powered By Prudour Pvt. Ltd.)
Email: inquiry@market.us
Address: 420 Lexington Avenue, Suite 300,
New York City, NY 10170, United States
Tel: +1 718 618 4351






















Comments
0 comment