views
Human Albumin Injection: Stop Shock, Start Stabilization
Human Albumin Injection: Stop Shock, Start Stabilization
Introduction: A Plasma-Derived Marvel in Modern Medicine
Human Albumin has firmly established itself as one of the most valuable and reliable biotherapeutics in critical and supportive care. Extracted and purified from human plasma, Human Albumin Injection is much more than just a volume expander—it is a life-saving therapeutic agent that plays an essential role in fluid resuscitation, oncotic pressure maintenance, and transport of various endogenous substances in the blood.
Across emergency rooms, ICUs, dialysis centers, and operation theaters, Human Albumin injection is trusted globally for managing hypovolemia, hypoalbuminemia, burns, and other acute clinical conditions. Due to its unmatched efficacy and natural origin, it continues to be a first-choice option when managing complex cases requiring plasma volume restoration or protein replenishment.
This comprehensive blog explores the science, benefits, uses, and clinical effectiveness of Human Albumin, providing valuable insights for healthcare providers, patients, and pharmaceutical professionals alike.
Table of Contents
- What is Human Albumin?
- Composition and Formulations
- Mechanism of Action: How It Works in the Body
- Indications and Medical Uses
- Dosage and Administration
- Clinical Effectiveness and Evidence
- Safety Profile and Side Effects
- Comparison with Alternatives
- Storage and Handling Guidelines
- Patient Benefits and Practical Considerations
- Expert Opinion and Global Usage
- Final Thoughts: Why Human Albumin Remains a Gold Standard
- Frequently Asked Questions (FAQ)
1. What is Human Albumin?
Human Albumin is a sterile, purified preparation of serum albumin protein derived from pooled human plasma. It constitutes about 60% of the total protein content in plasma and plays a vital physiological role in maintaining oncotic pressure and transporting hormones, fatty acids, and drugs. In clinical use, it is available as an injectable solution in varying concentrations—commonly 5%, 20%, and 25%.
Unlike synthetic volume expanders, Human Albumin is biologically compatible and does not carry the same risk of anaphylaxis or coagulopathy, making it an ideal candidate in many critical care settings.
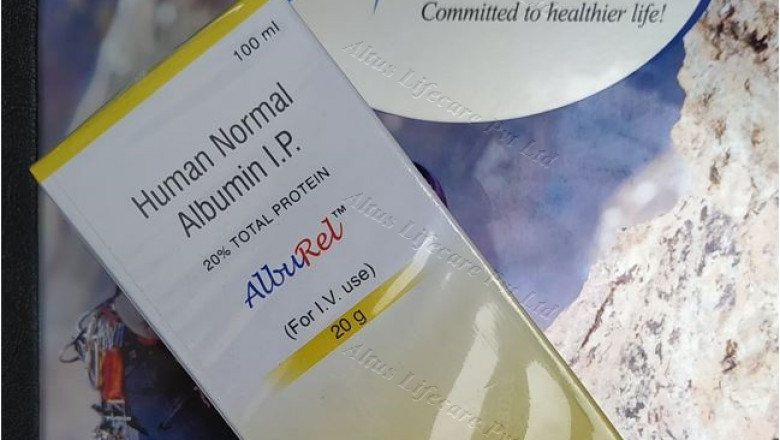
2. Composition and Formulations
Each vial of Human Albumin contains:
- Active Ingredient: Human Albumin (USP), typically 5 g, 20 g, or 25 g per 100 mL depending on concentration.
- Stabilizers: Sodium caprylate and sodium acetyltryptophanate to maintain stability and prevent aggregation.
- Sodium Content: Varies depending on concentration.
- pH Range: Generally maintained between 6.9 to 7.5.
Formulations are isotonic and heat-treated to inactivate potential viruses, ensuring high levels of safety and purity for patient use.
3. Mechanism of Action: How It Works in the Body
Human Albumin’s therapeutic value lies in its unique physiological roles, particularly its ability to maintain plasma oncotic pressure and serve as a versatile transport protein. These capabilities make it a central player in managing fluid imbalances and supporting systemic homeostasis in critically ill or hypoalbuminemic patients. Let’s dive deeper into its multifaceted mechanism of action:
1. Restoration of Plasma Oncotic Pressure
At the heart of Human Albumin’s mechanism is its role in exerting colloid osmotic pressure—also known as oncotic pressure. Albumin molecules are large and remain within the blood vessels after administration. These proteins create an osmotic gradient that draws water from the interstitial and intracellular compartments back into the vascular space.
This fluid shift has profound implications in emergency and critical care settings:
- Rapid correction of hypovolemia
- Stabilization of blood pressure
- Improved tissue perfusion
- Reduced risk of organ hypoperfusion
Unlike crystalloids, which quickly leak into tissues, Albumin remains intravascular for longer durations, ensuring more effective and sustained volume expansion.
2. Transport of Endogenous and Exogenous Substances
Albumin also functions as a carrier protein, binding to a variety of molecules in the bloodstream. These include:
- Endogenous substances like bilirubin, free fatty acids, calcium, and hormones (e.g., thyroxine, cortisol)
- Exogenous substances such as drugs (warfarin, phenytoin), making them more bioavailable and stable in circulation
This binding capability:
- Enhances pharmacokinetics and bioavailability
- Prevents toxic accumulation of free, unbound compounds
- Plays a buffering role in metabolic and pharmacological pathways
This unique transport functionality is critical, especially in patients with chronic liver disease or renal dysfunction, where natural albumin levels are severely depleted.
3. Antioxidant and Anti-inflammatory Effects
Emerging research highlights Albumin’s role in neutralizing reactive oxygen species (ROS) and modulating inflammation. By acting as a natural antioxidant, Albumin protects vascular endothelium and cellular structures from oxidative damage—a key contributor to disease progression in sepsis, ARDS, and trauma.
Furthermore, Albumin:
- Binds endotoxins, helping detoxify the bloodstream in infections
- Modulates the immune response by interacting with cytokines and immune cells
- Reduces capillary leakage by stabilizing endothelial junctions
This positions Albumin as not just a supportive therapy, but also a therapeutically active agent with disease-modifying potential in critically ill populations.





















Comments
0 comment