
Grocery Stores in Yuma, AZ: Where the Southwest Shops F...
Grocery Stores in Yuma, AZ: Where the Southwest Shops Fresh
-


Grocery Stores in Yuma, AZ: Where the Southwest Shops Fresh

Why Selling Your Car with Sell Your Car to Rob is the Easiest Way to Get Ri...

Why Selling Your Car Has Never Been Easier: Introducing Sellyourcar2rob

This beginner’s guide will walk you through everything you need to know abo...

Why Selling Your Car is a Hassle and How to Make it Easy
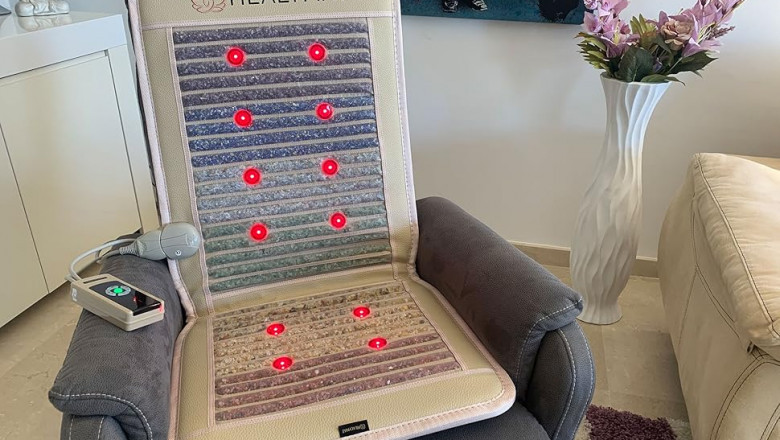
Kristallmatte für dein Wohlbefinden: Wie die Vital-Mat Körper und Geist unt...

Learn how to find the Best Butt Fat Transfer Surgeon in Dubai for a success...

Learn how to choose the Best Fat Transfer Surgeon in Dubai, including cost,...

